‘What is the difference between an Osteopath and a Chiropractor?’
A frequently asked question for many Osteopaths.
There are a handful of similarities between the two professions, but also differences in terms of their philosophy, patient assessment and the way they treat patients. And it’s useful to understand how each operates when you are considering treatment.
The philosophy of Osteopaths
Osteopaths deal with the whole body.
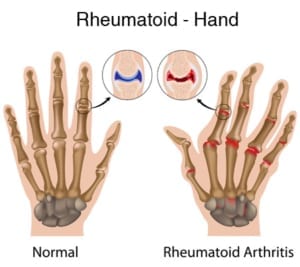
They take on a more holistic approach, treating musculoskeletal disorders relating to muscles, ligaments, joints, nerves, cartilage, tendons and the general skeletal system.
They also identify underlying, causative factors. So, Osteopathy can not only help to heal specific conditions but also work towards improving your overall health.
Osteopaths will consider where the root cause of your problem may be originating. For example, a patient may be suffering with facial pain, but this could be stemming from a problem in their neck. Which is, in turn, related to the function of the upper back, which is dependent to some extent on the biomechanics of their lower back. And their lower back is linked to the pelvic area – so they could be suffering with possible issues in their knees or feet.
Osteopath Robin Kiashek, who has more than 25 years’ experience said: “To help my patients understand the difference, I encourage them to think about house subsidence. London’s housing stock is built on clay, and during the hot summer months it is not uncommon to find the older properties developing cracks in the upper floors. One option is to fill in the cracks every year. But the problem is to do with ground movement below the house.
“Therefore, to solve the problem once and for all, Osteopaths generally address those underlying factors. In other words, they will, of course, fill in the cracks. But they will also address the movement below the house.”
The philosophy of Chiropractors
Chiropractors primarily focus on the spine.
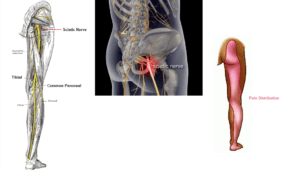
Generally speaking, Chiropractors believe that spinal misalignment is the root cause of their patient’s back symptoms. The spinal cord is simply an extension of the brain, and according to chiropractic belief, slight misalignment of a vertebra will affect the spinal nerves coming off the spinal cord.
Chiropractors believe that manipulation of the displaced vertebra, will address the spinal nerve compression and hence associated muscle or organ involvement.
Assessment with Osteopaths
At the initial consultation, Osteopaths will take a case history of the patient’s problem. This is followed by a physical examination during which they will ask the patient to undergo various movements in a bid to reproduce their symptoms.
The Osteopath will use a combination of visual analysis and touch (or palpation) to understand the problem at hand. They may also use orthopaedic tests and occasionally refer for further x-ray or MRI investigation to help form a diagnosis.
Once a diagnosis has been reached, an Osteopath will give the patient a full explanation and a treatment plan. A treatment will be included in the initial Osteopathic consultation, assuming it is safe to do so.
The treatment plan will let the patient know what aggravating factors to avoid and will include lifestyle advice to help them do so.
Assessment with a Chiropractor
At a Chiropractor’s initial consultation, they will usually come to diagnosis from the use of x-rays, focussing largely on the spinal integrity. On the second visit, the patient will be informed of the Chiropractor’s diagnosis and on the third visit, treatment will commence.
Treatment: what to expect with an Osteopath
After the initial consultation, treatment will begin, and most Osteopaths will then see patient once a week for half an hour.
Treatments may include gentle soft tissue release through massage, joint mobilisation and gentle conservative spinal manipulation. In addition, Robin Kiashek may use a range of allied therapies including Western Medical Acupuncture and Low Level Laser Therapy.
Treatment: what to expect with a Chiropractor
Chiropractors are more well known for focusing on the spinal adjustments or clicking which may not be as gentle as Osteopathic treatment. The Chiropractor will focus primarily on the lower and upper back and neck.
Chiropractors tend to see their patients ‘little and often’. Treatments themselves normally last around 15 minutes. But they may see their patients two to three times a week.
A final word from Robin
Robin added: “In addition to the difference between Osteopathy and Chiropractic outlined above, it’s important to remember that each Osteopath and Chiropractor will practice in their own unique way. They may have particular specialisms or areas of interest. So, don’t’ be afraid to do your research – practitioners will be more than happy to answer your questions.”
If you are in pain or have any questions about how Osteopath, Robin Kiashek, could be of benefit, then please get in touch. Osteopaths are deemed as essential workers. Therefore, they can continue to treat patients through lockdown and patients are permitted to seek medical help. Robin Kiashek is fully compliant with Government regulations re PPE.






![sciatica_diagram [Converted]](https://www.robinkiashek.co.uk/wp-content/uploads/2018/12/sciatica_diagram-Converted-251x300.jpg)
 Here at the Robin Kiashek Clinics we promote prevention, and have plenty of advice on keeping your spine healthy and pain-free (
Here at the Robin Kiashek Clinics we promote prevention, and have plenty of advice on keeping your spine healthy and pain-free (
 Massage is good for so many aspects of your health. Primarily it helps increase endorphins – your body’s natural painkillers – that provide relief to sufferers of chronic pain. It helps stimulate your circulation, bringing a good blood supply to the affected area, and it improves your lymphatic drainage system helping your body combat disease.
Massage is good for so many aspects of your health. Primarily it helps increase endorphins – your body’s natural painkillers – that provide relief to sufferers of chronic pain. It helps stimulate your circulation, bringing a good blood supply to the affected area, and it improves your lymphatic drainage system helping your body combat disease.