Someone once mentioned to me that “we are the sum total of the decisions we make in life” Did you see Chelsea Cameron on Victoria Derbyshire’s show when she thanked her drug-dependent parents for all the things they DIDN’T do for her as a child and the choices she made subsequently?:
http://www.bbc.co.uk/news/uk-38825332
With this in mind, my wife Georgie and I found ourselves last year at a craft exhibition in London. Whilst we were looking for a particular exhibitor, we came across the work of Peter Lanyon who was exhibiting his woodcraft furniture in one of the stalls (www.peterlanyonfurniture.co.uk).
Rewinding the clock nearly 50 years, one of the few subjects I enjoyed at school, apart from Biology, was woodworking but being a boy and it being the 1970s, science was the obvious avenue to pursue.

Magazine rack made at school, circa 1973
I was taken by Peter’s beautiful handmade Devon furniture, which uses coppiced wood i.e. freshly cut unseasoned Greenwood and traditional woodworking tools. On the spur of the moment, I signed up with my wife to do Peter’s ‘Introduction to Greenwood Furniture Making’ for my 60th birthday present!

Shaping the Ash legs from a split tree trunk
Whilst this was relatively familiar territory for me, for Georgie it was very much out of her comfort zone. So why mention this in my newsletter to you? The answer I believe is that as we all become older, so we become more set in our ways, both emotionally and physically. For most of my patients and our society generally, lives are largely sedentary and much like me, one gravitates towards what is most comfortable and familiar.


It is interesting I find how conquering one’s own, seemingly trivial, mental limitations can have profound and far-reaching results in one’s lives. My wife, who is a primary school teacher, had an OFSTED-type class inspection the following week after her return from Peter’s course. She claims that her ‘Outstanding’ OFSTED result was, in part, due to the positive emotional influence she felt having conquered her reservations of her own ability to do woodcraft.

The finished products (Georgie’s table left)
So my message to everyone is: DO SOMETHING DIFFERENT! It needn’t be doing a course – I sometimes ride my motorbike to work a different way …. it’s very small and trivial but it’s just “doing something different”. When was the last time you spontaneously said “hello” to a stranger in an elevator? How often do you stop to say “hello” to someone living rough? And so the list goes on and on. In NLP jargon, it’s called “changing state”.
 The push for Evidence Based Medicine seems to be a double edged sword – without a double blind trial supporting a claim of efficacy, as required by The Advertising Standards Authority (ASA), one is unable to make claims for a treatment of any condition a patient may be suffering. With costly research, Osteopathy is lagging behind the ‘firepower’ of well-funded pharmaceutical companies.
The push for Evidence Based Medicine seems to be a double edged sword – without a double blind trial supporting a claim of efficacy, as required by The Advertising Standards Authority (ASA), one is unable to make claims for a treatment of any condition a patient may be suffering. With costly research, Osteopathy is lagging behind the ‘firepower’ of well-funded pharmaceutical companies. You may remember that I recently wrote about the BBC programme The Doctor Who Gave Up Drugs. Along similar lines I recently attended a workshop based on Cure: A Journey Into the Science of Mind over Body which is a bestselling book by Jo Marchant.
You may remember that I recently wrote about the BBC programme The Doctor Who Gave Up Drugs. Along similar lines I recently attended a workshop based on Cure: A Journey Into the Science of Mind over Body which is a bestselling book by Jo Marchant. Episode one is the first of a two-part social experiment in which Doctor Chris van Tulleken takes over part of a GP surgery and stops patients’ prescription pills. Here is a link to the program, which can be found on BBC iPlayer:
Episode one is the first of a two-part social experiment in which Doctor Chris van Tulleken takes over part of a GP surgery and stops patients’ prescription pills. Here is a link to the program, which can be found on BBC iPlayer:  Twenty years later, Doctor Tulleken’s fascinating two-part program illustrates how people suffering with, what he would describe as lifestyle illnesses can gradually begin to be weaned off their medication (with their GPs guidance); these patients suffer from a variety of different conditions including long-term chronic lower back pain, depression and hypertension, to name a few.
Twenty years later, Doctor Tulleken’s fascinating two-part program illustrates how people suffering with, what he would describe as lifestyle illnesses can gradually begin to be weaned off their medication (with their GPs guidance); these patients suffer from a variety of different conditions including long-term chronic lower back pain, depression and hypertension, to name a few.![sciatica_diagram [Converted]](https://www.robinkiashek.co.uk/wp-content/uploads/2018/12/sciatica_diagram-Converted-251x300.jpg)
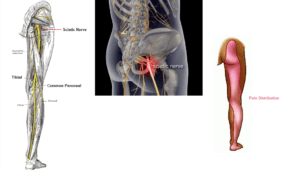 Here at the Robin Kiashek Clinics we promote prevention, and have plenty of advice on keeping your spine healthy and pain-free (
Here at the Robin Kiashek Clinics we promote prevention, and have plenty of advice on keeping your spine healthy and pain-free (